Fertility treatment 2023: trends and figures
Preliminary UK statistics for IVF and DI treatment, storage, and donation
Published: June 2025
You have chosen not to allow videos from the 3rd party streaming service (YouTube), if you would like to see these videos, please change your Privacy policy and cookie settings.
Download the underlying dataset as Excel Worksheet
Table of contents
- Main points
- Note on preliminary data
- Section 1: More babies born from IVF in the UK
- Section 2: IVF pregnancy and birth rates using fresh embryo transfers increased over the years, though lower for Black patients
- Section 3: Average pregnancy and birth rates using frozen embryo transfers increased in 2023
- Section 4: Multiple births rate from IVF is one of the lowest in the world
- Section 5: Most treatment types have increased across the UK since 2019
- Section 6: Increased number of patients with female partners and single patients in 2023
- Section 7: NHS-funded cycles varied by nation and English region
- About our data
Main points
- In 2023, 52,400 patients had over 77,500 in vitro fertilisation (IVF) cycles at licensed fertility clinics in the UK.
- Babies born from IVF increased from about 8,700 in 2000 to 20,700 in 2023.
- IVF births are making up a higher proportion of all UK births over time, increasing to over 3% in 2023 from less than 1.5% in 2000, around 1 in 32 UK births – roughly one IVF child in every classroom.
- In 2023, 11% of all UK births to those aged 40-44 were a result of IVF, increasing from 4% in 2000 and accounting for 0.5% of all UK births.
- In 2023, around 820 babies were born following donor insemination (DI) treatment.
- Births from donor treatments made up around 1 in 5 of all IVF and DI births in 2023, accounting for around 1 in 153 of all UK births.
- The average IVF pregnancy rate using fresh embryo transfers increased nationally to 31% per embryo transferred in 2023, with the highest pregnancy rate among patients aged 18-34 at 41%.
- The preliminary average IVF birth rate using fresh embryo transfers was 25% nationally, with 35% for patients aged 18-34 and 5% for patients aged 43-44 when using their own eggs in 2023.
- In 2023, the average pregnancy rate using frozen embryo transfers was 39% per embryo transferred and the average preliminary birth rate was 33% per embryo transferred.
- Multiple births from IVF have continued to fall to 3.4% in 2023, one of the lowest rates in the world.
- Total treatment and storage cycles increased from 86,000 in 2019 to nearly 99,000 in 2023.
- Egg freezing cycles increased from 4,700 in 2022 to 6,900 in 2023, accounting for 7% of all cycles. Egg freezing increased most among patients in their 30s, but the number of patients using their stored frozen eggs in treatment remains low.
- Single patients increasingly used both IVF and DI from 2019 to 2023, particularly in IVF use (+83%).
- The average proportion of National Health Service (NHS) funded IVF cycles declined from 35% in 2019 to 27% in 2023 in the UK, decreasing most in England.
- National differences in the proportion of NHS-funded IVF cycles continued, ranging from 24% in England, 33% in Wales, to 49% in Northern Ireland and 54% in Scotland in 2023.
Note on preliminary data
This report provides an update on fertility treatment and outcomes in the UK from 1991 to 2023. Due to large-scale work to upgrade the HFEA data submission system and migrate data to a new database, data on treatments and pregnancies from 2020-2023 and outcomes from 2019-2023 have not yet been validated.I This means that some data in this report is preliminary and cannot be compared to other reports. Data validation is expected to be complete in Winter 2025/26.
The HFEA dashboard shows HFEA data from 1991 onwards and is interactive, allowing users to investigate the topics in this report in more detail. Clinic level data can be found on Choose a Fertility Clinic.
1. More babies born from IVF in the UK
In 2023, 52,400 patients had over 77,500 IVF cycles at licensed fertility clinics in the UK. About 20,700 babies were born as a result of IVF in 2023, increasing from 8,700 in 2000.
IVF births are making up a higher proportion of all UK births over time, increasing from 1.3% in 2000 to 3.1% in 2023 (Figure 1). This means around 1 in 32 UK births in 2023 were via IVF – roughly one child in every classroom – compared to 1 in 43 in 2013.
The relative contribution of IVF to national births varies across Europe. Approximate percentages of IVF births range from 11% in Denmark in 2021, to 5% in Belgium and 3% in France in 2019.1-2, II The differences between countries are complex and can be explained by a combination of socio-cultural, demographic, economic and policy factors, including the availability of state-funding for fertility treatment.
In 2023, 2,900 patients had about 5,500 donor insemination (DI) cycles. DI births accounted for around 820 babies born in the UK – 0.1% of all UK births.
Around 1 in 5 of all IVF and DI treatment births in the UK, 4,300 births, were a result of treatment using donor eggs, sperm or embryos. When comparing to all UK births, donor treatment births accounted for around 1 in 153 of all births and have continued to increase since 2008, with most using donor sperm.
Figure 1. Number of IVF births have increased over time
Number of IVF births in the UK by donation use, 2000-23
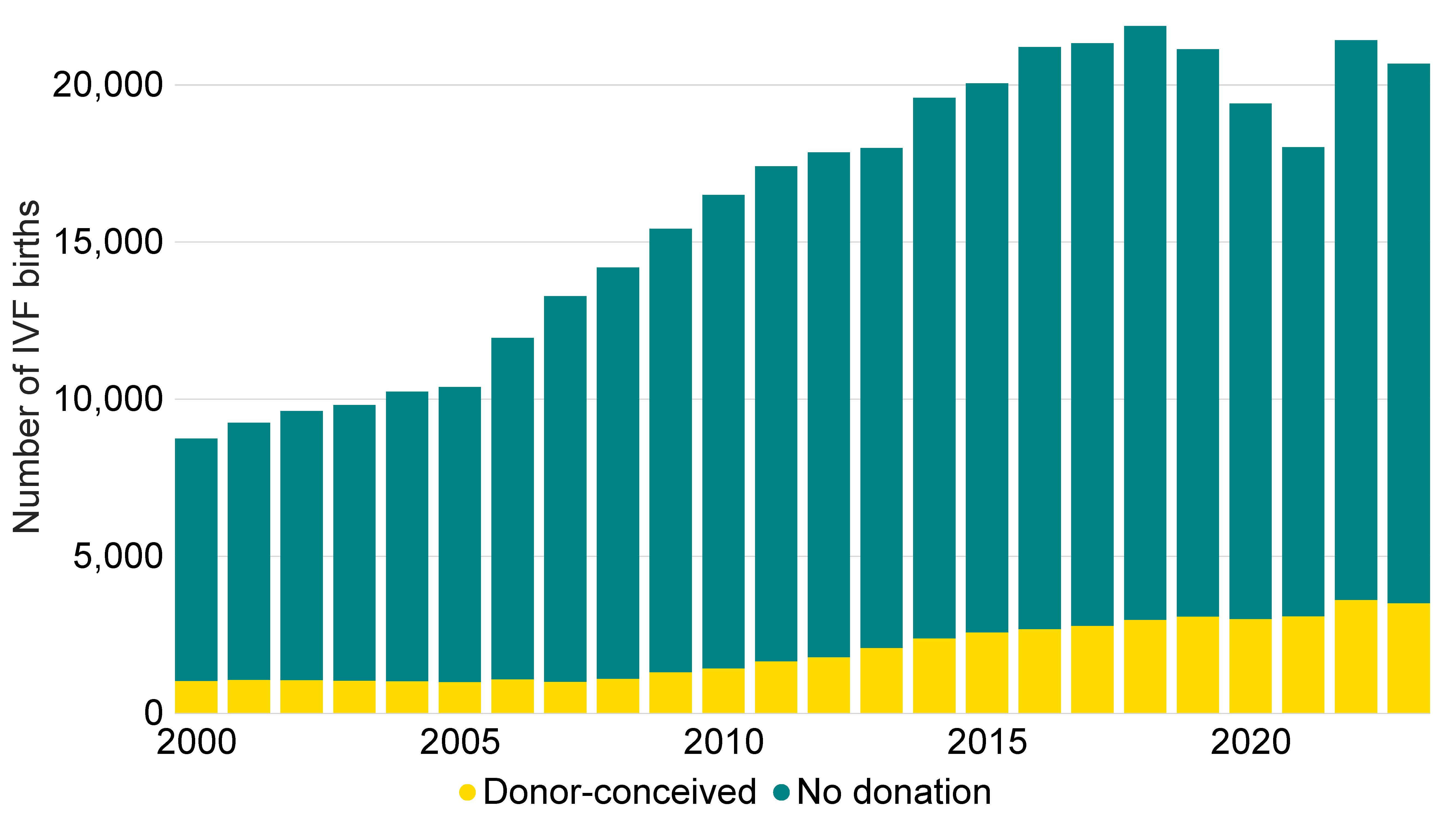
Note figure 1: The IVF live birth data for 2019-23 is preliminary and has not been validated. The drop in 2020 and 2021 is likely due to the decreased treatment activities in 2020 during the COVID-19 pandemic.3 Year refers to the year of birth, rather than year of treatment. All births submitted to the HFEA as a result of fertility treatment undertaken in the UK licensed clinics are included regardless of patients’ residence and may include births that occurred outside of the UK. National birth data is from the Office for National Statistics,4 National Records of Scotland,5 and Northern Ireland Statistics and Research Agency.6
Download the underlying data for Figure 1 as Excel Worksheet
Most births in the UK are among those aged under 35 (75%). The proportion of births as a result of fertility treatment increases with age (Figure 2). Around 2% of births (7,949) among those under 35 were a result of IVF in 2023, an increase from 1% in 2000. For patients aged 40-44, there were 3,486 births from IVF, which is 11% of all babies born in the UK to those in this age group – a rise from 4% in 2000.
The average age patients started IVF in 2023 was around 35 years old, similar to 2022. Most patients (83%) started IVF treatment under 40 years old and 17% started at 40 years or over in 2023. As birth rates decline with age (see section 2) and NHS funding is less common for patients aged over 40, earlier treatment can increase the chances of success.
Figure 2. 11% of all UK births to those aged 40-44 were a result of IVF
Proportion of IVF births of all live births in the UK by age group, 2000 and 2023
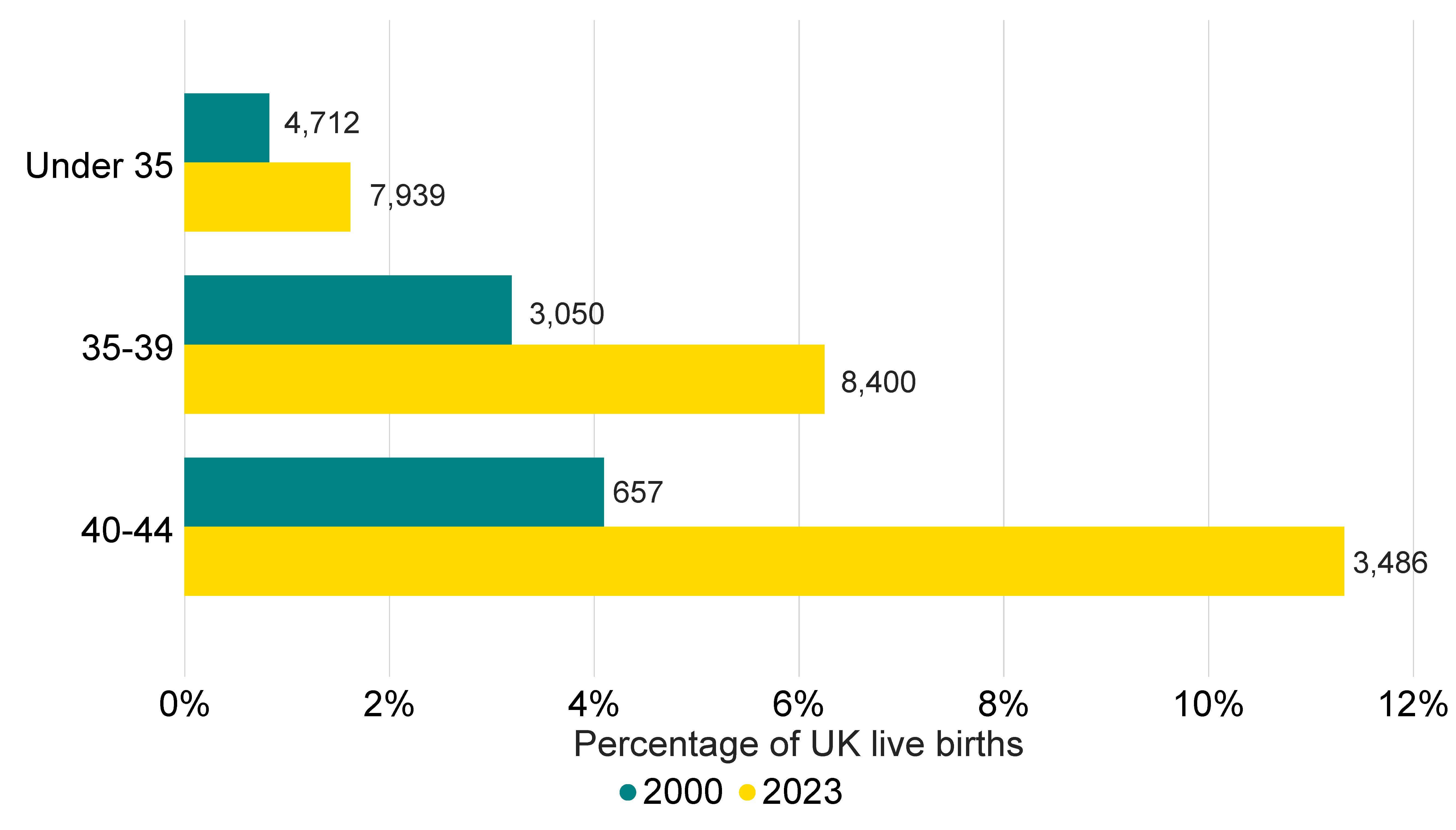
Note figure 2: The IVF live birth data for 2023 is preliminary and has not been validated. Numbers refer to total IVF births occurred in that year. Year refers to the year of birth, rather than year of treatment. Age refers to age at birth, rather than age at treatment. All births submitted to the HFEA as a result of fertility treatment undertaken in the UK licensed clinics are included regardless of patients’ residence and may include births that occurred outside of UK. National birth data is from the Office for National Statistics,4 National Records of Scotland,5 and Northern Ireland Statistics and Research Agency.6
Download the underlying data for Figure 2 as Excel Worksheet
2. IVF pregnancy and birth rates using fresh embryo transfers increased over the years, though lower for Black patients
The average overall pregnancy rate from IVF using fresh embryo transfers and patient’s own eggs increased from 22% per embryo transferred in 2013 to 31% in 2023. Patients aged 18-34 had the highest pregnancy rate per embryo transferred at 41% in 2023 (Figure 3). Pregnancy rates per embryo transferred increased from 24% in 2013 to 34% in 2023 for patients aged 35-37, and from 18% to 25% for patients aged 38-39. For patients aged 43-44 pregnancy rate per embryo transferred increased when using their own eggs from 6% in 2013 to 9% in 2023.
Rising pregnancy rates for all age groups are likely to relate to improved clinical and laboratory practice. The declining success rates with age highlight the importance of early referrals to gynaecological care and fertility clinics, as well as speaking to a general practitioner (GP) as soon as possible if patients are having difficulty getting pregnant.7
Figure 3. IVF pregnancy rate using fresh embryo transfers increased over the years
Average fresh embryo transfer IVF pregnancy rate per embryo transferred using patient eggs by age group, 1991-2023
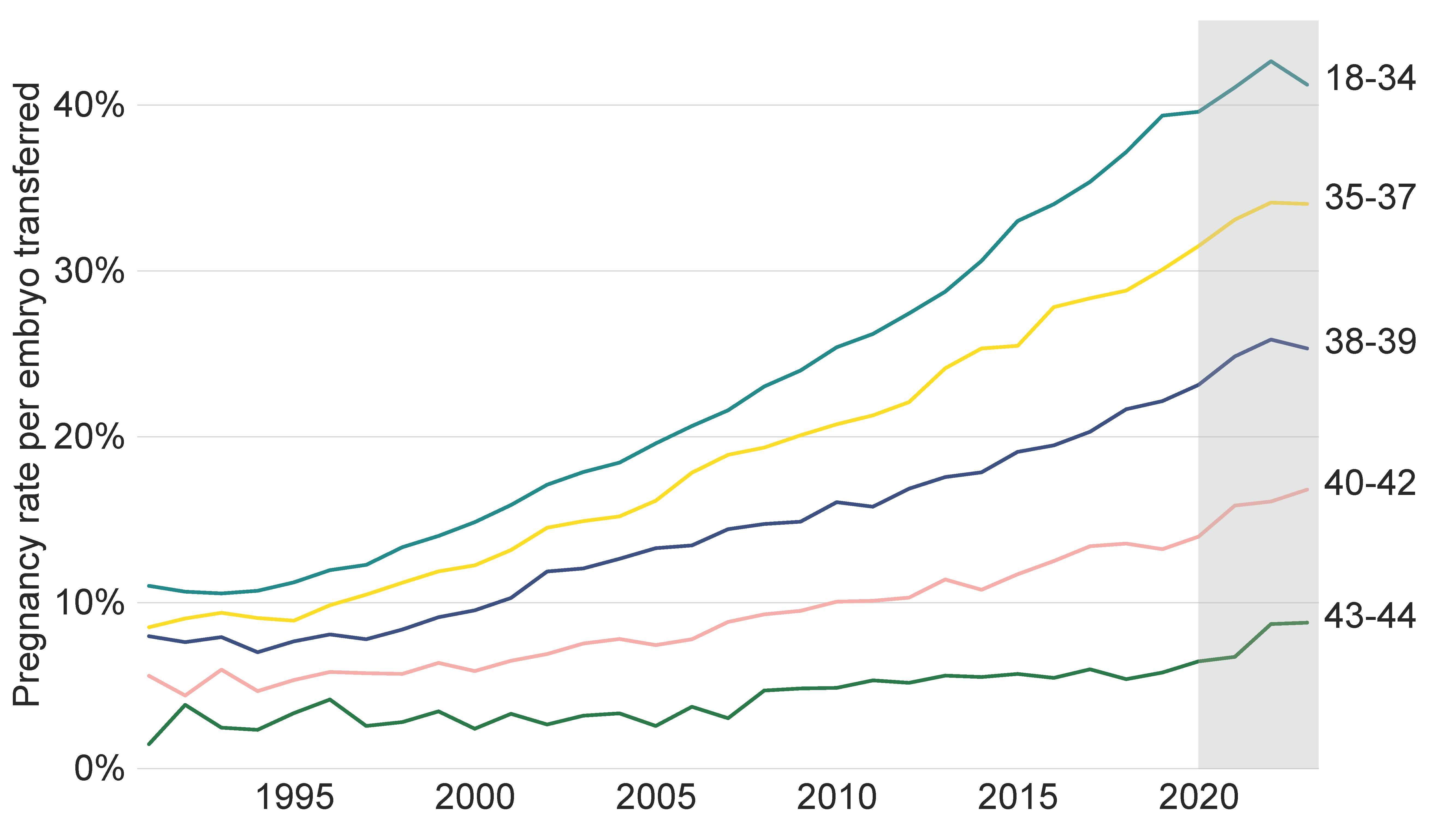
Note figure 3: Pregnancy rates per embryo transferred for 2020-23 are preliminary and have not been validated (grey band). This data includes IVF treatment cycles using their own fresh egg and fresh embryo transfers, and begun with the intention of immediate treatment, instead of storing eggs or embryos for future use. Treatments using previously stored eggs, PGT-A/M/SR, donor eggs or surrogacy have been excluded. Pregnancy rates from 2020-23 may be underestimated and may increase from the current estimates following data validation.I
Download the underlying data for Figure 3 as Excel Worksheet
The average birth rate from IVF using fresh embryo transfers and patient’s own eggs increased from 19% per embryo transferred in 2013 to 25% in 2023 (Figure 4). We suggest using pregnancy rates as an indicator for progress in recent years as ongoing data validation work with clinics is likely to mean birth rates from 2019 to 2023 are currently underestimated.
While the birth rates have remained similar since 2019, patients aged 18-34 had the highest birth rate per fresh embryo transferred at 35% in 2023 and patients aged 43-44 had the lowest at an average of 5% in 2023. Although birth rates have increased steadily over the past three decades, treatment outcomes vary by ethnicity and family types.8-9
Birth rates have been shown in our Ethnic diversity in fertility treatment reports to be lower among Black patients. In 2022-23, the average birth rate per embryo transferred for Asian and Black patients aged 18-37 was 27% and 25% respectively, compared to 33% for White patients and 30% for patients from a mixed ethnic background. See the HFEA dashboard for further information by ethnicity.
Figure 4. IVF birth rate using fresh embryo transfers similar since 2019
Average fresh embryo transfer IVF birth rate per embryo transferred using patient eggs by age group, 1991-2023
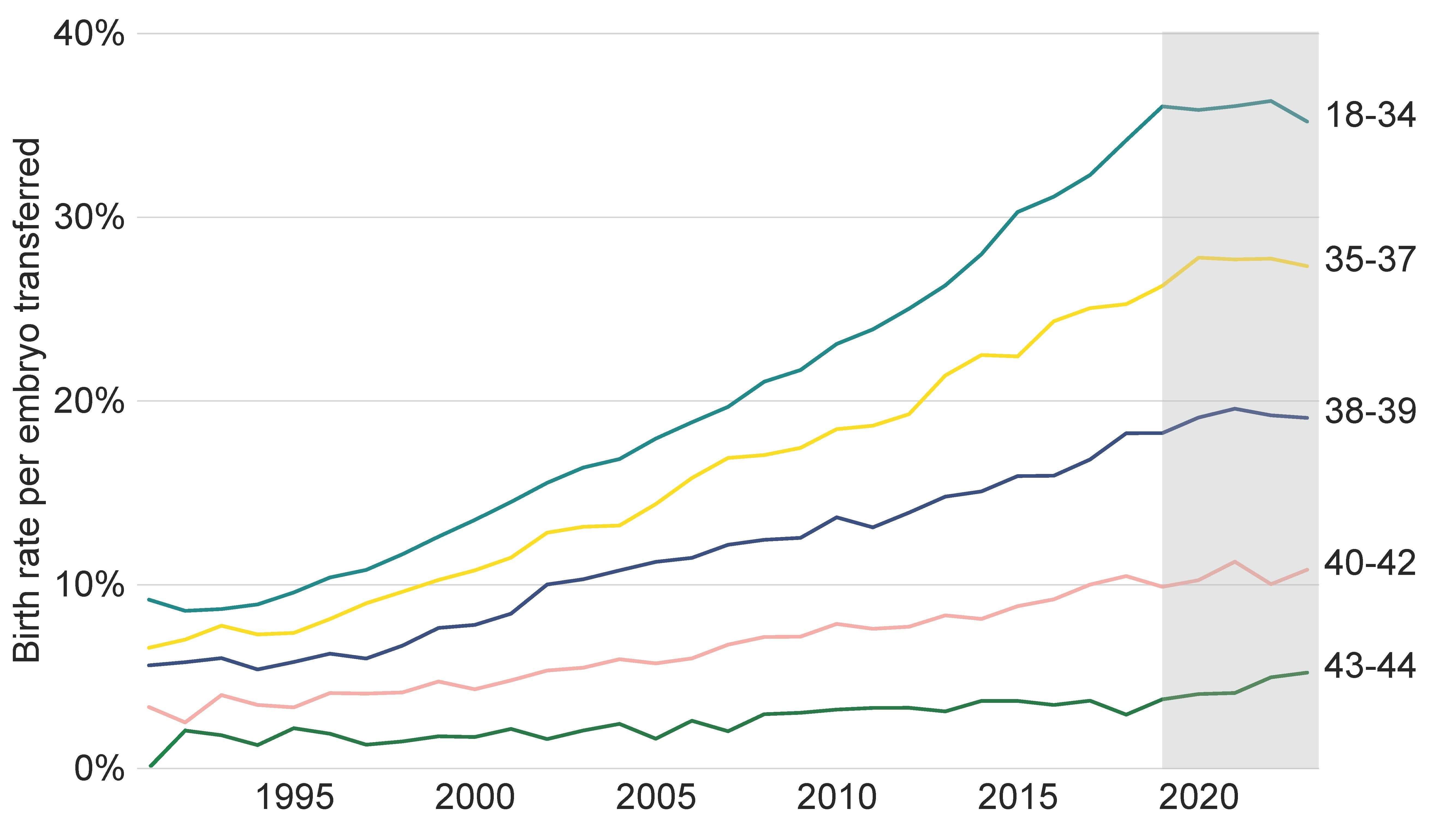
Note figure 4: Birth rates per embryo transferred for 2019-23 are preliminary and have not been validated (grey band). This data includes IVF treatment cycles using their own fresh eggs and fresh embryo transfers, and begun with the intention of immediate treatment, instead of storing eggs or embryos for future use. Treatments using previously stored eggs, PGT-A/M/SR, donor eggs or surrogacy, and treatments in which a pregnancy but no birth outcome was recorded have been excluded. Birth rates from 2019-23 may be underestimated due to missing outcome data and are expected to increase from the current estimates following data validation.I
Download the underlying data for Figure 4 as Excel Worksheet
3. Average pregnancy and birth rates using frozen embryo transfers increased in 2023
The improved freezing techniques from the late-2000s means a typical IVF patient today will have a single fresh embryo transferred in their first cycle, and any additional embryos frozen for later use. The number of frozen embryo transfer cycles has more than doubled from 2013 to 2023, accounting for 45% of all embryo transfers in 2023.
The average pregnancy rate using frozen embryo transfers increased from around 20% in 2013 to 39% in 2023 (Figure 5). Importantly, the average birth rate using frozen embryo transfers increased, in line with pregnancy rates, from around 18% in 2013 to 33% in 2023. The higher pregnancy and birth rates from frozen transfers may be partly because only embryos with sufficient quality for transfer are stored for later use. When using frozen embryo transfers, pregnancy and birth rates are largely related to the age of the patient at egg collection rather than age at embryo transfer.
Figure 5. Pregnancy and birth rates using frozen embryo transfers increased in 2023
Average frozen embryo transfer pregnancy and birth rates per embryo transferred using patient eggs, 1991-2023
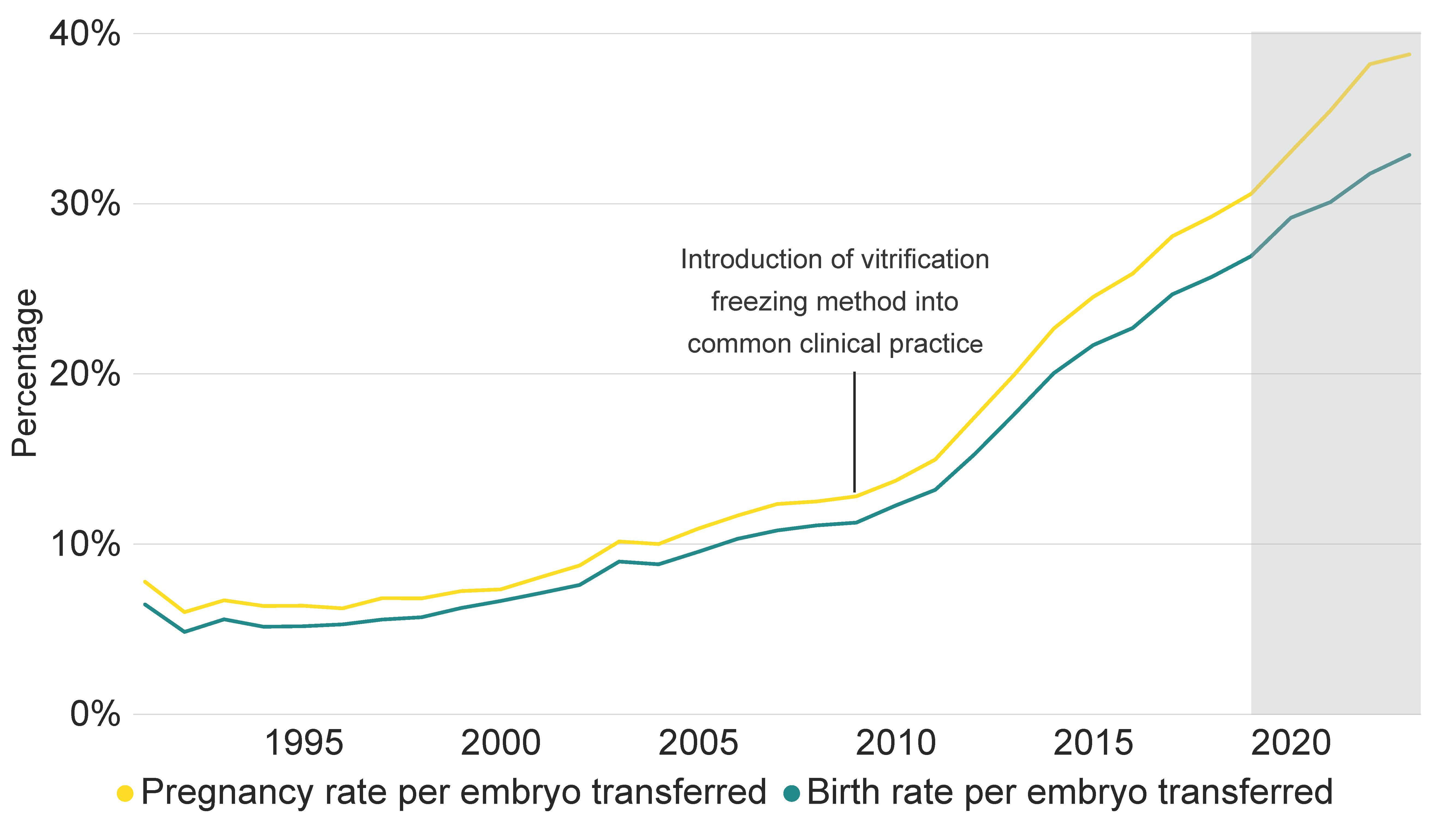
Note figure 5: Pregnancy rates for 2020-23 and birth rates for 2019-2023 are preliminary and have not been validated (grey band). This data includes IVF treatment cycles using their own eggs and frozen embryo transfers, and begun with the intention of immediate treatment, instead of storing eggs or embryos for future use. Treatments using previously stored eggs, PGT-A/M/SR, donor eggs or surrogacy, and treatments in which a pregnancy but no birth outcome was recorded have been excluded. Pregnancy rates from 2020-23 and birth rates from 2019-23 may be underestimated due to missing outcome data and are expected to increase from the current estimates following data validation.I
Download the underlying data for Figure 5 as Excel Worksheet
4. Multiple births rate from IVF is one of the lowest in the world
Multiple births have increased risk of health problems for patients and their babies, such as preterm birth, pre-eclampsia, and still birth, as well as neonatal and maternal death. There is also a significant cost saving to the NHS with the reduction in multiple births. A report in 2018 estimated that health care costs for twin births are, on average, almost three times as high as for singleton births.10
In the early 1990s the average UK multiple birth rate from IVF was around 28%, compared to 1-2% estimated in natural conception.11 Following the launch of the ‘One at a time’ campaign in 2007 and the introduction of a multiple birth rate target in the UK in 2009, the 10% target was reached in 2017.
The average multiple birth rate decreased to the lowest UK average of 3.4% in 2023 (Figure 6). This is among the lowest multiple birth rates in the world, similar to Sweden, Australia and New Zealand.12-13 Most clinics operate within the national average, with around 90% of clinics meeting the 10% multiple birth rate target in 2023.
Multiple births in IVF treatment are largely determined by the number of embryos transferred to the womb. Single embryo transfers increased from around 10% of IVF cycles in the early 2000s to 88% of IVF cycles in 2023. This has also led to the increased number of frozen embryo transfers, as single embryo transfers with later frozen embryo transfers have become common practice (See section 3 and 5).
Figure 6. Average IVF multiple birth rate reduced further to 3.4% in 2023
Average IVF multiple birth rate, 1991-2023
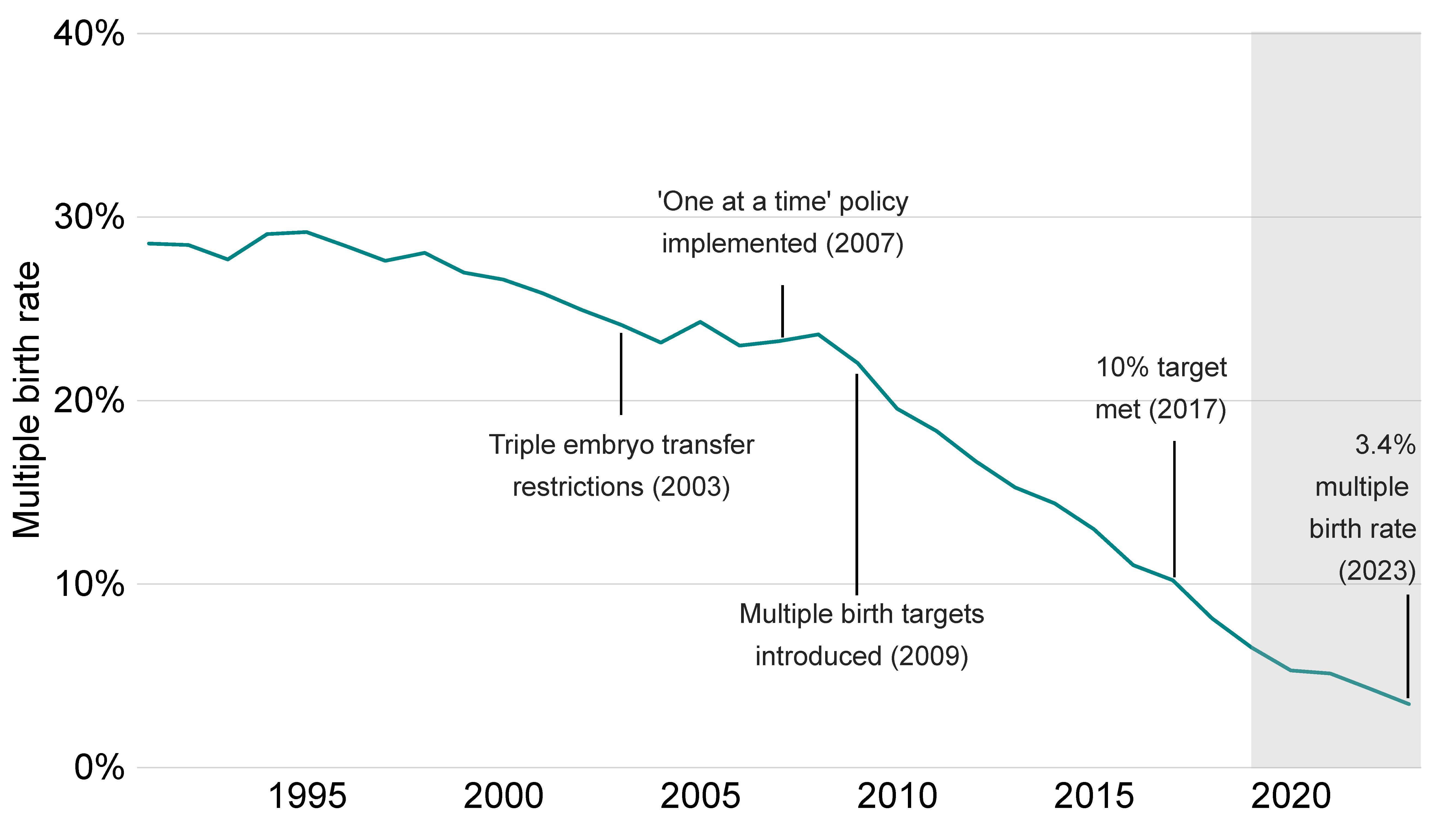
Note Figure 6: Multiple birth rates for 2019-23 are preliminary and have not been validated (grey band). This data includes cycles using either patient or donor eggs, either fresh or frozen embryo transfer, and IVF treatment cycles begun with the intention of immediate treatment, instead of storing eggs or embryos for future use. Treatments in which a pregnancy but no birth outcome was recorded have been excluded.
Download the underlying data for Figure 6 as Excel Worksheet
5. Most treatment types have increased across the UK since 2019
In 2023, around 98,900 treatment and storage cycles were undertaken in the UK. Most cycles were IVF treatments (78%), followed by embryo storage (9%), egg freezing (7%) and DI treatments (6%).
Fresh embryo transfer IVF increased by 3% and frozen embryo transfer cycles increased by 24% from 2019 to 2023 (Table 1). The larger increase in frozen embryo transfer is consistent with longer term trends and will be due in part to increased use of single embryo transfers over the last decade (see section 3).
DI cycles declined by 4% from 2019 to 2023. This is explained by the increased use of IVF over DI among all family types. See our Family formations in fertility treatment 2022 report for more details.
Egg freezing cycles increased from 2,567 in 2019 to 6,932 in 2023 (+170%), accounting for 7% of all cycles. Embryo storage increased from 8,190 in 2019 to 8,908 in 2023 (+9%).
The number of new egg donors slightly decreased from 1,495 in 2019 to 1,392 in 2023, while sperm donors increased by 18%. The increase in sperm donors mainly relates to the import of donor sperm from overseas sperm banks, which accounted for 70% of new sperm donors in 2023. The number of new UK sperm donors has remained similar in the past decade.
| Table 1. Frozen embryo transfer cycles increased by 24% since 2019 | ||||
|---|---|---|---|---|
| Number of cycles by intended activity and new egg and sperm donors, 2019-23 | ||||
| 2019 | 2022* | 2023* | % change 2019 to 2023 |
|
| IVF- fresh embryo transfer | 41,154 | 41,316 | 42,310 | +3% |
| IVF- frozen embryo transfer | 28,414 | 33,839 | 35,202 | +24% |
| DI | 5,752 | 5,645 | 5,505 | -4% |
| Treatment total | 75,320 | 80,800 | 83,017 | +10% |
| Embryo storage | 8,190 | 9,572 | 8,908 | +9% |
| Egg freezing | 2,567 | 4,688 | 6,932 | +170% |
| Storage total | 10,757 | 14,260 | 15,840 | +47% |
| New egg donors | 1,495 | 1,772 | 1,392 | -7% |
| New sperm donors | 841 | 1,030 | 992 | +18% |
| New donors total | 2,336 | 2,802 | 2,384 | +2% |
| Note table 1: The counts for 2022-23 are preliminary and have not been validated (*). This data does not include cycles carried out for the purposes of donation. This data uses new egg and sperm donor registrations only. Donors that registered multiple times will only be counted in the year of their first registration. | ||||
Download the underlying data for Table 1 as Excel Worksheet
Egg freezing cycles have increased across all age groups from 2019 to 2023, with the largest increases among patients aged 30-37 (Figure 7). Egg freezing increased from 1,200 cycles in 2022 to 2,000 in 2023 (+67%) among patients aged 30-34 and from 1,500 to 2,300 (+53%) among patients aged 35-37.
Data collected by the HFEA does not distinguish between reasons for storing eggs. However, we are able to estimate that at least 16% of egg freezing cycles were for medical reasons in 2018-22.8 Although there has been a big increase in the number of patients freezing their eggs for non-medical reasons in recent years, our data shows the number of those patients using their frozen eggs remains low.8 A patient’s chances of conception using frozen eggs depends on patient’s age at the time of freezing and how many eggs were frozen. Egg freezing is not a guarantee of having a baby in the future and it’s important to understand the risks and costs involved.
Figure 7. Egg freezing cycles increased most among patients in their 30s
Number of egg freezing cycles by age group at freezing, 2019-23
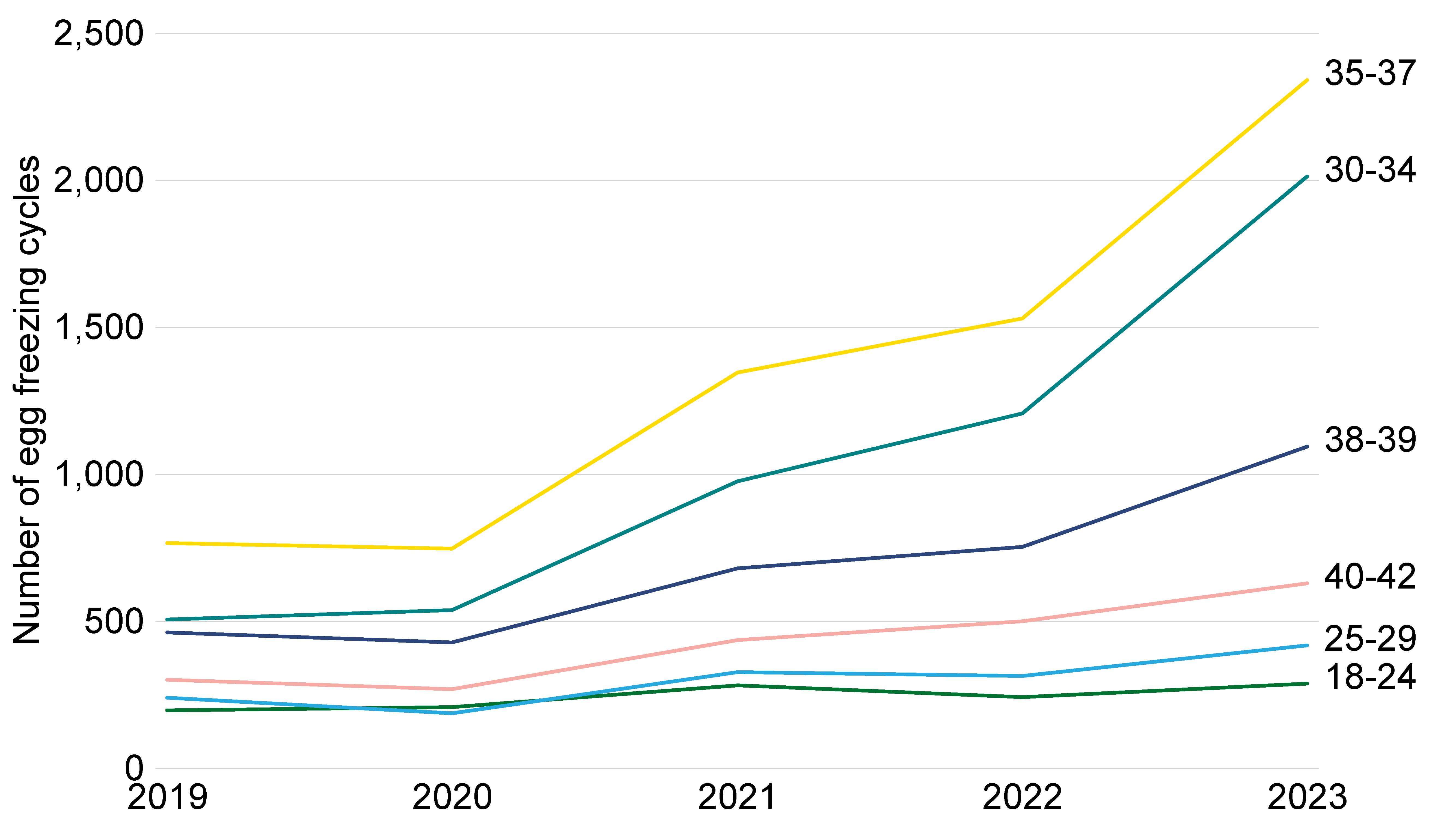
Note figure 7: The data for 2020-23 is preliminary and has not been validated. This data excludes cycles where eggs/embryos were stored and donated in the same treatment.
Download the underlying data for Figure 7 as Excel Worksheet
6. Increased number of patients with female partners and single patients in 2023
Opposite-sex couples accounted for 89% of all IVF patients in 2023 and the patient number increased slightly from 2019. The number of female same-sex IVF patients increased from 1,761 to 2,559, and single IVF patients increased from 2,021 in 2019 to 3,693 in 2023 (Table 2).
Single patients accounted for the largest proportion of patients undergoing DI (48%) in 2023 and the patient number increased by 16% from 2019 to 2023, while there was a 40% decline among opposite-sex couples undergoing DI.
There is a general trend shifting from DI to IVF among all family types. In addition, the increased use of IVF among female same-sex couples will in part relate to use of reciprocal IVF.III See section 5 and Family formations in fertility treatment 2022 report.
The number of surrogates decreased from 267 in 2019 to 233 in 2023, which accounted for less than 1% of all patients.
| Table 2. Female same-sex and single IVF patients increased by at least 45% since 2019 | ||||
|---|---|---|---|---|
| Number of patients by treatment and family type and surrogacy, 2019 and 2023 | ||||
| 2019 | 2023* | % change 2019 to 2023 |
||
| IVF | Opposite-sex couple | 46,181 | 46,429 | +1% |
| Female same-sex couple | 1,761 | 2,559 | +45% | |
| Single patient | 2,021 | 3,693 | +83% | |
| Surrogacy patient | 267 | 233 | -13% | |
| DI | Opposite-sex couple | 506 | 305 | -40% |
| Female same-sex couple | 1,336 | 1,280 | -4% | |
| Single patient | 1,195 | 1,389 | +16% | |
| Note table 2: The data for 2023 is preliminary and has not been validated (*). Number of patients is a distinct count. This means if a patient underwent two cycles in the same year they would be counted once. If they underwent a cycle in 2019 and then again in 2023, they would be counted once in each of these years. Includes patients undergoing treatment where the cycle was begun with the intention of immediate treatment, instead of storing eggs or embryos for future use. The IVF data includes cycles using either fresh or frozen embryo transfer. Data on intended parents is not available on the Register. | ||||
Download the underlying data for Table 2 as Excel Worksheet
7. NHS-funded cycles varied by nation and English region
NHS funding for IVF cycles varies considerably across the UK depending on national or local funding criteria. Overall, NHS-funded IVF cycles decreased from 35% in 2019 to 27% in 2023 in the UK, remaining the same as in 2022 (Figure 8).
In 2023, Scotland had the highest proportion of NHS-funded IVF cycles at 54% compared to 49% in Northern Ireland, 33% in Wales and 24% in England. NHS-funded cycles increased in Northern Ireland from 2019 to 2023, while decreasing most in England.
In Scotland, Wales and Northern Ireland, the level of NHS funding is set nationally. Funding decisions in England are made by Integrated Care Boards (ICBs), though the National Institute for Clinical Excellence (NICE) provides recommended access criteria.14-15 NHS-funded IVF varied considerably across English regions, ranging from 51% in the North East to 20% in London and 18% in the South East and East Midlands in 2023.
The decrease in NHS-funded IVF treatments across the UK may relate to increased waiting times for further investigations prior to accessing NHS-funded treatments.16 Changes in national and regional funding criteria both in the devolved nations and across Integrated Care Boards (ICBs) in England may have also had an impact on the number of NHS-funded IVF cycles.
Figure 8: NHS-funded IVF cycles decreased from 35% in 2019 to 27% in 2023
Proportion of IVF cycles funded by the NHS in UK nations and English regions, 2019 and 2023
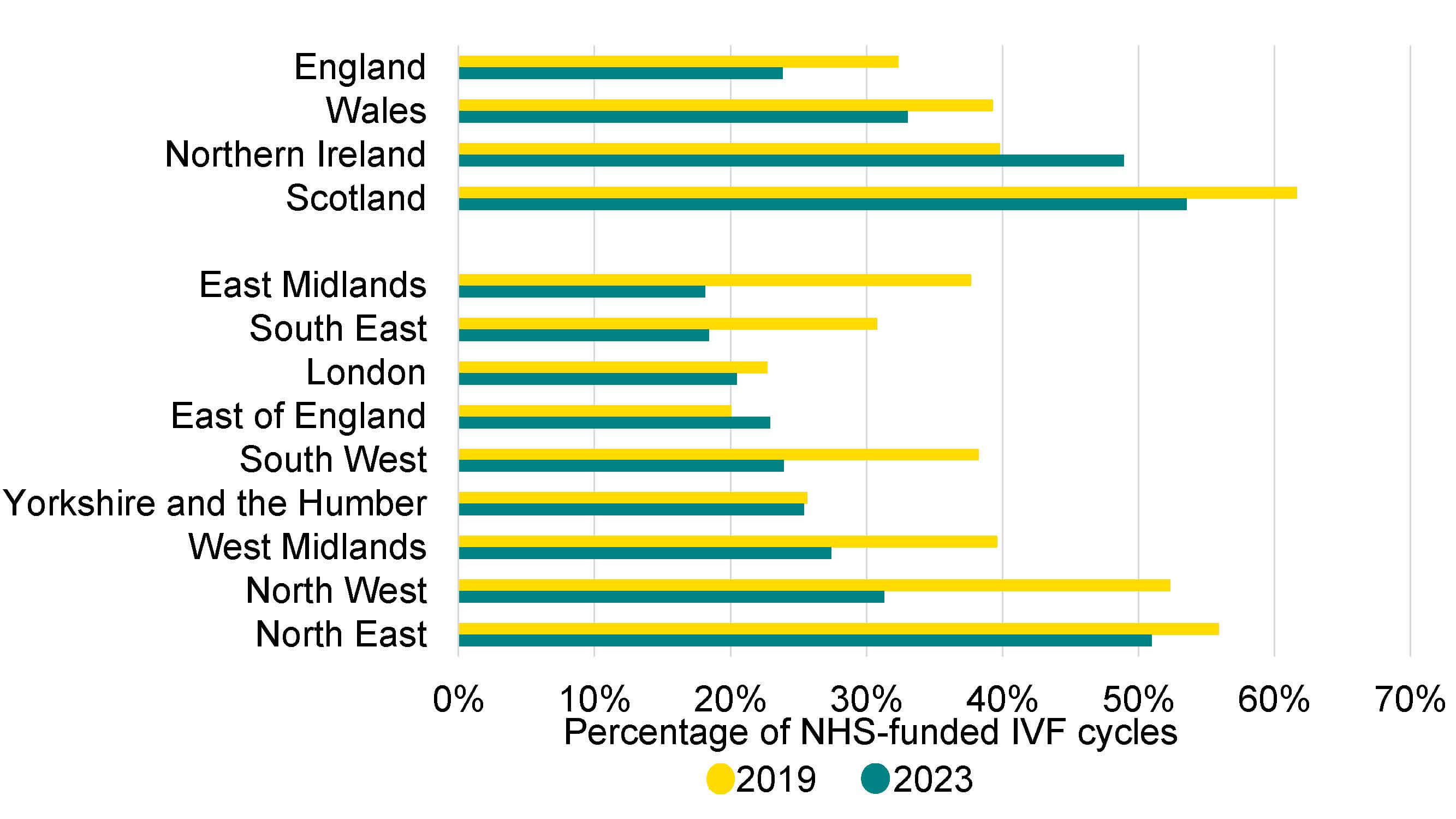
Note figure 8: The data for 2023 is preliminary and has not been validated. This data includes IVF treatment cycles begun with the intention of immediate treatment, instead of storing eggs or embryos for future use, using either fresh or frozen embryo transfer. Nation and region is based on clinic location, rather than patient’s residence.
Download the underlying data for Figure 8 as Excel Worksheet
About our data
This report covers the period from 1991-2023 where data is available. Data for 1991 covers a partial year, starting in August 1991. The information that we publish is a snapshot of data provided to us by licensed clinics as required by the Human Fertilisation and Embryology Act 1990. Data from one clinic is excluded due to data reporting issues. Averages used are provided as mean values unless stated otherwise. The data used in this report is from the Register as of 1 May 2025. Results are published according to the year in which the cycle was started.
This report uses preliminary treatment and pregnancy data for 2020-2023 and preliminary birth outcome data for 2019-2023. This is because the HFEA has recently launched a new data submission system for licensed clinics and migrated our fertility treatment and outcomes data to a new database. This data migration has resulted in delays, which has prevented the validation of the 2020-2023 treatment and pregnancy data and 2019-2023 birth outcome data. Because of this, these statistics cannot be classified as official statistics. Data validation involves data quality checks that verify treatment, pregnancy and birth outcome data. Data validation is expected to be complete by Winter 2025/2026.
For further information, please see our Quality and Methodology report.
About the HFEA
The HFEA is the UK’s independent regulator of fertility treatment and research using human embryos. Set up in 1990 by the Human Fertilisation and Embryology Act, the HFEA is responsible for licensing, monitoring, and inspecting fertility clinics and research centres – and taking enforcement action where necessary – to ensure everyone accessing fertility treatment receives high quality care.
The HFEA is an ‘arm’s length body’ of the Department of Health and Social Care, working independently from Government providing free, clear, and impartial information about fertility treatment, clinics and egg, sperm, and embryo donation.
The HFEA collects and verifies data on all treatments that take place in UK licensed clinics, which can support scientific developments and research and service planning and delivery.
The HFEA is funded by licence fees, IVF treatment fees and a small grant from UK central government. For more information, visit hfea.gov.uk.
Contact us regarding this publication
Media: press.office@hfea.gov.uk
Statistical: intelligenceteam@hfea.gov.uk
Accessibility: comms@hfea.gov.uk
Footnotes
- Data validation involves quality checking data submitted from licensed clinics across the UK to that verify treatment, pregnancy and birth outcome data is correctly recorded on our data Register.
- These proportions may be calculated using number of births from IVF cycles in the year of treatment, rather than births that occurred in the year. There may be other differences in the calculation and definition of births from the UK data presented in this report.
- Reciprocal IVF (also known as ‘shared motherhood’ or ‘shared parenthood’) is where eggs are collected from one partner in a same-sex female or other LGBTQIA+ couple and fertilised with donor sperm. The resulting embryo is then transferred into the other partner’s womb, who carries the pregnancy.
Notes on fertility treatment 2023: preliminary trends and figures
- Danish Fertility Society. Annual report 2021. 2023.
- European IVF Monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE); Smeenk J, Wyns C, De Geyter C, Kupka M, Bergh C, Cuevas Saiz I, De Neubourg D, Rezabek K, Tandler-Schneider A, Rugescu I, Goossens V. ART in Europe, 2019: results generated from European registries by ESHRE. Human Reproduction. 2023.
- Human Fertilisation and Embryology Authority (HFEA). Impact of COVID-19 on fertility treatment 2020. 2022.
- Office for National Statistics (ONS). Births in England and Wales: birth registrations, 2023. Released 28 October 2024.
- National Records of Scotland. Vital Events Reference Tables 2023. Released 30 July 2024.
- Northern Ireland Statistics and Research Agency. Registrar General Annual Report 2023, Birth 2023 Tables. Released 21 November 2024.
- Human Fertilisation and Embryology Authority (HFEA). National Patient Survey 2024. 2025.
- Human Fertilisation and Embryology Authority (HFEA). Family formations in fertility treatment 2022. 2024.
- Human Fertilisation and Embryology Authority (HFEA). Ethnic diversity in fertility treatment 2021. 2023.
- National Guideline Alliance, Royal College of Obstetricians and Gynaecologists (RCOG). A report by the National Guideline Alliance about twin pregnancy costing. 2018.
- Monden C, Pison G, Smits J. Twin Peaks: more twinning in humans than ever before. Human Reproduction. 2021.
- National Quality Registry for Assisted Reproduction (Q-IVF). Fertility treatments in Sweden National report 2023: Results and trends 2021. 2023.
- Newman JE, Kotevski DP, Paul RC, Chambers GM. 2024. Assisted reproductive technology in Australia and New Zealand 2022. Sydney: National Perinatal Epidemiology and Statistics Unit, the University of New South Wales.
- Department of Health and Social Care (DHSC). Guidance: NHS-funded in vitro fertilisation (IVF) in England. Updated 1 February 2024.
- National Institute for Clinical Excellence (NICE). Fertility problems: assessment and treatment. Updated 6 September 2017.
- Royal College of Obstetricians and Gynaecologists (RCOG). Waiting for a way forward. 2025.
| Publication date: |
|---|

