World Embryologist Day in the life: “I love to perform transfers as it can be a really exciting and hopeful time for the patient.”
In celebration of World Embryologist Day, Georgina shares a typical day in the life of an embryologist and what she enjoys about working in an embryology lab.
The IVF lab is run by a team of embryologists every day, each with different roles and responsibilities. Ensuring everything gets done is a team effort that requires everyone to have eyes on what is going on in the lab and remain flexible to help others where required.
Morning (8am-11:30am)
The beginning of the day is usually very busy. An embryologist grades embryos, to check their quality and viability, and calls patients with day 1 fertilisation results and day 5, 6, and 7 embryo development updates. We freeze and transfer at the blastocyst stage, the stage of embryo development which occurs between days 5 and 7. These embryos contain hundreds of cells, and the distinct structures that will go on to form the baby and the placenta are visible. We gain consent for freezing with or without biopsy (for pre-implantation genetic testing), which is confirmed to the embryologist who will perform this throughout the day.
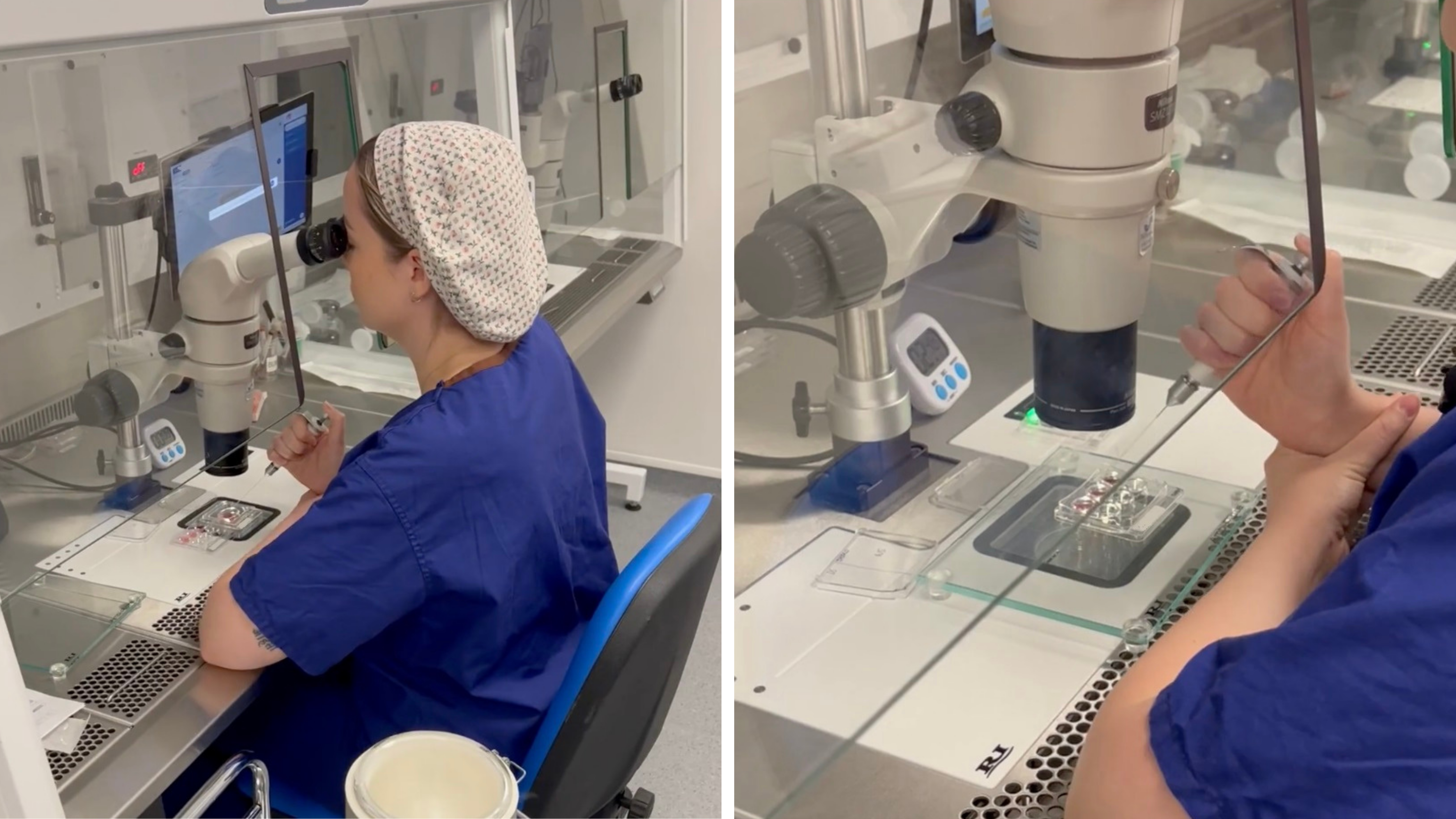
If the transfer of a frozen embryo is taking place, the embryo must be thawed at least two hours before transfer. When embryos are frozen, they collapse down into a tight ball. When we thaw them, we like to see that the cells have survived, and that the embryo has started to re-expand into its shell. Thawing early gives us flexibility to call the patient and discuss thawing a second embryo if we don’t see this happening, although this is rare. An embryologist will assist in transfer by loading the embryo into the catheter and aiding the doctor with passage through the cervix. I love to perform transfers as it can be a really exciting and hopeful time for the patient, and I enjoy discussing embryos face-to-face!
Patient egg collections also take place in theatre early in the morning, and the attending embryologist will confirm the treatment plan with the patient going forwards. This happens while partner or donor sperm is prepared in the lab.
We’re here for you, so don’t be afraid to speak to us if you have any concerns or queries about the process – we want to make sure you’re as informed as possible about what will happen to your eggs, sperm, and embryos.
Midday (11:30am-2:30pm)
We like to see how the sperm looks and moves to determine whether it is suitable for conventional IVF insemination or intracytoplasmic sperm injection (ICSI), which is often done by semen analysis before the day of egg collection. Conventional IVF insemination is where we place eggs and sperm into the same dish overnight. In ICSI, the embryologist picks the most morphologically normal sperm and injects one into each suitable egg. This is very time-sensitive, so we need to make sure that this is done approximately four hours after egg collection.
Our embryo grader performs embryology consultations around midday. These dedicated slots allow patients to individually discuss their upcoming treatment cycle. We describe the laboratory aspects of the patient’s cycle, explain our treatment recommendations, and allow the patients to ask any questions they may have. We find this really helps with patient understanding in an area that likely feels very foreign, and it hopefully helps to build trust in the embryology team as we are very aware of the huge role we have in their cycle.
Afternoon (2:30pm-4:00pm)
An important aspect of afternoon work is preparing for the clinical procedures the following day. This involves writing up patient treatment plans, checking that all the correct consents are in place, and ensuring that virology blood results are acceptable. Once this is completed, dishes are prepared for the following day. Many dishes and media tubes need to be incubated overnight so that the media balances to a suitable temperature and pH for eggs, sperm, and embryos. All dishes and tubes are tagged with radiofrequency identification tags and labels displaying three patient identifiers. This allows electronic and manual witnessing to prevent mismatches. All procedures in our laboratory are witnessed using the electronic witnessing system, and critical, irreversible steps are double witnessed by two staff members. The electronic system will alarm if two different patients are brought into the workspace, which significantly reduces risk.
I’m currently in my third and final year of the embryologist training course (Scientist Training Programme, STP). My main goal moving forward is to be trained on ICSI within the next few months. When patients consent for training on their unused gametes and embryos, it means that I can learn how to do essential processes within the laboratory. We never train on gametes or embryos that could be used clinically, and there are processes in place to ensure this doesn’t happen. Training for ICSI involves learning how to inject bubbles into eggs and practising sperm immobilisation and aspiration. In the latter, we strike the sperm tail which halts sperm movement and causes a reaction that aids fertilisation. Then, we can aspirate the sperm up the injection pipette and practice movement control. This allows me to improve my technique before I start injecting eggs with sperm for clinical use. My colleagues and I are very grateful to the patients that donate their unused gametes and embryos for training purposes, it is an incredibly selfless donation that facilitates the embryology training programme.

About the author:
Georgina is a Trainee Embryologist at The Evewell West London, completing her final year of training on the Scientist Training Programme (STP). Georgina attended Newcastle University for her undergraduate degree in Biomedical Sciences (BSc) and Master’s degree in Medical Genetics (MRes). Georgina held a number of laboratory technician positions before being accepted onto the STP in 2022, through which she is also undertaking a part-time Master’s degree in Embryology (MSc) at Manchester Metropolitan University.
| Publication date: |
|---|

